What is anal incontinence?
Anal incontinence is the loss of stool control and inability to defer defecation to reach a restroom. The inability of control bowel movements causes feces to leak unexpectedly. Anal incontinence impacts both genders although it is more common in women. Some studies estimate that approximately 10 to 15% of the world population is affected by this condition. Anal incontinence negatively impacts the quality of life and leads to social isolation, embarrassment, and depression.
What causes anal incontinence?
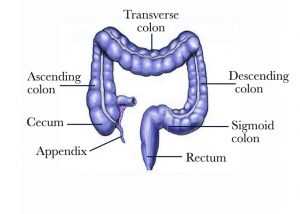
Incontinence of feces can be triggered by weak anus and pelvic floor muscles [Figure 1], and/or abnormal function of the large bowel including the colon and rectum [Figure 2].

Figure 1 – Pelvic organs including the anus, pelvic muscles, and the rectum
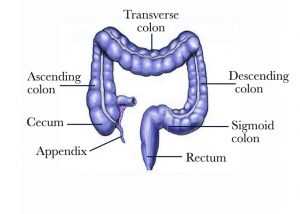
Figure 2 – The large bowel including the colon and the rectum
Common causes of fecal incontinence include any of the following conditions:
- Aging
- Cancer
- Childbirth injuries (tear, episiotomy, forceps delivery)
- Constipation with large hard stool or fecal impaction
- Dementia or memory loss
- Diabetes
- Diarrhea
- Inflammatory bowel disease
- Irritable bowel syndrome
- Laxative use
- Neurologic disorders (conditions that affect the nerves)
- Prior anal or proctologic surgery
- Prior pelvic surgery
- Radiation to the pelvis
- Rectal prolapse (the rectum falling out through the anus)
- Rectocele
- Spinal cord injury
- Stroke
What are the symptoms of anal incontinence?
Patients with anal incontinence can present with a spectrum of symptoms that vary from mild to disabling severity and of various frequency and duration. Some patients may present immediately after a triggering event such as a traumatic childbirth or several decades later. Patients may have passive incontinence (spontaneous occurrence with or without awareness of the patient), urge incontinence (patient inability to defer defecation when trying to reach the bathroom), or a mixed pattern. Anal incontinence can lead to the inability to hold gas, liquid, solid stool, or a mixed pattern. In its milder form, the incontinence may occur on rare occasions when the stool is liquid in nature but in some cases, the patient can experience daily leakage. Most patients with significant symptoms wear a pad or a diaper to protect the skin and the clothes.
How is the patient with anal incontinence evaluated?
The most important part of the evaluation is the history provided by the patient and the office-based examination performed by Dr. Maher Abbas. A determination of the possible causes of the incontinence is possible in most patients based on the history. The type and severity of the incontinence is quantified using a clinical scale that measures the frequency of the episodes, type, and severity. Visual inspection of the exterior aspect of the pelvis and anus, a brief testing of the sensation, an evaluation of the muscle, and Anoscopy is performed to check the inside of the anus. In addition, several tests are helpful in assessing the function of the anus and pelvic muscles. They include:
-
Blood tests: thyroid hormone and calcium level, C-reactive protein (CRP). These tests are helpful in patients with large bowel conditions
-
Imaging studies: An endoanal ultrasound to look at the anal muscles or alternatively an MRI scan of the pelvis to assess the anus and pelvic floor muscles. In patients with abnormal defecation, a dynamic MRI (magnetic resonance imaging) defecography to check for pelvic floor function. During this procedure, gel material is inserted into the rectum and in some cases the vagina. MRI pictures are obtained at rest and when the patient tries to defecate. This test provides the opportunity to visualize the internal pelvic organs in action
-
Procedures: Flexible sigmoidoscopy or Colonoscopy to visualize the inside of the rectum and colon. Anorectal manometry with testing of rectal compliance and a balloon expulsion test to evaluate the anal sphincter muscle function. Pudendal nerve testing and anal electromyography (EMG) can evaluate the function of the nerve supply to the anus.
What treatment options are available for anal incontinence?
Medical Treatment
Most patients with anal incontinence can be successfully treated medically. Surgical intervention is an option for patients with severe incontinence and those patients who do not respond to initial medical therapy. Medical treatment consists of several options including the following:
-
Avoidance of gut stimulants. Patients who use laxatives for regularity maybe triggering anal incontinence. Reducing or eliminating the regular use of laxatives is advisable. Increasing dietary fiber or adding a fiber supplement can be a good alternative for most patients. Avoidance of sugar free gums [which contain stimulants like sorbitol] or magnesium supplements is another important measure
-
Dietary modifications. The patient is advised to maintain a diet and bowel diary for a couple of months to identify triggering factors and food products that improve the symptoms. Recording the daily intake and bowel function (number and consistency of the stool, episodes of leakage) is important. A review of a properly maintained diary can provide valuable information for dietary modification
-
Lifestyle modifications. For some patients having a bowel movement the same time every day, using the toilet right before leaving the house, carrying protective supplies (panty liners, pads) and an extra change of clothing are some of the ways to cope with anal incontinence
-
Physical therapy. Biofeedback/Kegel Exercises strengthen the anus and pelvic floor musculature. A prolonged course of daily therapy is needed for a minimum of 2 to 3 months to see a significant effect. Working with a physical therapist specialized in pelvic floor disorders is very important
-
Rectal enemas or irrigation. The cleansing of the rectum with an enema or rectal irrigation can provide the patient with a several hour window of clean bowel and minimizes the chances of anal incontinence
-
Regulating bowel motions. Both constipation and diarrhea can worsen or trigger anal incontinence. Avoidance of either loose or hard stools can be beneficial to the patient. Relieving Constipation with increasing dietary fiber consumption, fiber supplements, the judicious use of laxatives, and a higher fluid intake is customized based on the patient’s degree of constipation. Treating or eliminating the cause of diarrhea is an important aspect of medical therapy. The use of anti-diarrheal medications such as Imodium (loperamide hydrochloride) should be titrated to the degree of the patient’s symptoms. This medication is best taken 30 minutes prior to a meal
-
Skin protection. The skin around the anus is sensitive and it can become irritated from feces. Keeping the skin dry and using moisture barrier creams, non-medicated talcum powder or cornstarch is helpful. After washing the skin around the anus, it is better to air-dry or pat dry the area with a clean washcloth rather than wiping with rough toilet paper. Patients who have significant irritation can use a zinc oxide-based ointment to protect and heal the skin. Patients who develop a yeast related rash do benefit from a brief course of antifungal cream. The use of a pad or diaper in patients with severe incontinence is advisable.
Surgical Treatment
Several surgical interventions are available to treat patients with severe incontinence and those patients whose symptoms are not controlled with medical therapy. The type of intervention is personalized based on various factors. Dr. Maher Abbas will recommend what is best for you. The following are the various options currently available:
-
Anal sphincter repair. A tear in the anus can be repaired using a technique called sphincteroplasty and levatorplasty. The damaged ends of the sphincter and pelvic floor muscles are reconstructed in an overlapping fashion to re-establish continuity and strength
-
Artificial bowel sphincter. The use of a silicon based or a magnetic ring like device can be used to encircle the patient anus to provide more support. The silicon based artificial sphincter is currently not available on the market and the magnetic device is still under scientific investigation
-
Colostomy. Diverting the stool to the skin of the abdomen is an option reserved only for patients with severe incontinence that does not respond to the various types of medical and surgical therapy. The use of colostomy is very rare as most patients can be treated successfully with other interventions
-
Implantable devices. This type of new technology is one of the most effective way to restore muscle tone and continence. A device is implanted in the buttock area and a thin wire stimulates the pelvic floor musculature. Patients with urinary incontinence can benefit
-
Injectable bulking agents. The injection of a paste like material into the anal area can add bulk to the anus and improve incontinence. This procedure is a minimally invasive procedure that is a good option for patients with a focal defect in the anus and passive type incontinence
-
Posterior tibial nerve stimulation (PTNS). The use of a thin needle similar to an acupuncture needle can be used to stimulate the posterior tibial nerve just above the inner aspect of the ankle. The stimulation is done on weekly basis for several months and would need to be repeated for long-term relief
-
Rectal repair. Patients with Rectal prolapse or Rectocele can benefit from surgical correction of these defects which often contribute to anal incontinence.
Why seek care with Dr. Maher Abbas?
Dr. Maher Abbas is American Board Certified in Colon and Rectal Surgery with special interest in anal incontinence and pelvic floor disorders. He provides the entire spectrum of operations including minimally invasive surgery and the latest technologies such as Implantable devices for incontinence.

If you would like to schedule a consultation with Dr. Maher Abbas to discuss and evaluate your condition, click here. If you have previously undergone any operation or tests related to your condition, kindly bring all outside reports for Dr. Maher Abbas to review the day of your consultation.