What is ulcerative colitis?
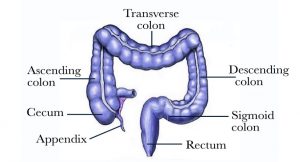
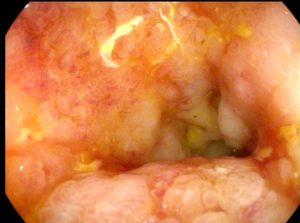
Ulcerative colitis is a condition which causes inflammation of the large bowel (colon and rectum) [Figure 1]. The lining of the bowel becomes inflamed and scarred [Figure 2]. Some patients can develop inflammation in other parts of the body such as the bone joints, spine, eyes, liver, and skin. Ulcerative colitis can appear at any age with some patients presenting early in life before age of 40 and some later in life between age 60 and 70 years. Both men and women are affected equally by this condition. The exact cause of ulcerative colitis is unknown but an immune system over response to some environmental exposure such as food or bacteria is thought to be a potential cause. A family history is present in some patients.
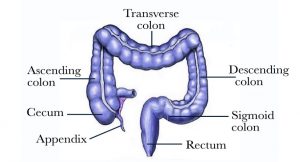
Figure 1 – The large bowel
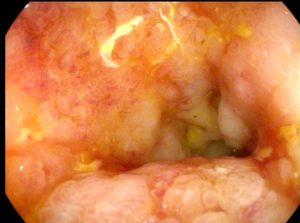
Figure 2 – Colonoscopy view of the rectum shows severe inflammation in a patient with ulcerative colitis
What are the symptoms of ulcerative colitis?
The symptoms and clinical findings of ulcerative colitis can vary from mild to severe and include one or more of the following:
- Abdominal pain and cramping
- Anemia
- Blood in the stool
- Diarrhea
- Eye inflammation
- Fatigue
- Fever
- Inflammation of the liver and bile ducts
- Joint inflammation
- Lack of appetite and weight loss
- Skin rash
How is ulcerative colitis diagnosed?
Dr. Maher Abbas will assess your symptoms and perform a physical examination before recommending specific tests to either diagnose ulcerative colitis or to assess severity of inflammation. Helpful tests include:
- Blood tests: CBC (complete blood count to test for anemia or infection), CRP (C reactive protein) and ESR (erythrocyte sedimentation rate) to assess degree of inflammation, thyroid function tests, liver and kidney function tests, tests for hepatitis virus and tuberculosis
- Imaging studies: computed tomography scan (CT) and/or magnetic resonance imaging (MRI) are special radiological studies to look inside the abdomen and pelvis. A variation of both scans is enterography which utilizes special techniques to look specifically at the small intestine. Enterography is recommended if there is any suspicion for the other type of inflammatory bowel disease called Crohn’s Disease
- Procedures: Colonoscopy is a procedure which allows Dr. Maher Abbas to look inside the large bowel including the colon and rectum
- Stool tests: calprotectin level (to assess for degree of inflammation in the intestine), clostridium difficile bacteria toxin, FOBT (fecal occult blood test)
How is ulcerative colitis treated?
Ulcerative disease is a chronic condition that requires long-term care. The majority of patients respond to medical therapy. Several medications are currently effective in controlling the symptoms of ulcerative colitis. They include oral pills, intravenous or subcutaneously injected medications, rectal liquid enemas, and anal suppositories.
Surgical intervention is reserved for a minority of patients whose symptoms are not controlled with medications, those who cannot tolerate the side effects of the medications or require high dose prednisone, and patients who develop precancerous or cancerous lesions in the colon and rectum. Most patients who require surgery need to have the colon and rectum removed with the construction of a small intestine pouch (ileal pouch) connected to the anus. In most patients, a 2-stage operation is performed with the use of a temporary Ileostomy which is typically closed within few months. On rare occasions, a permanent ileostomy is needed. Patients who present an as emergency require an initial operation to remove the colon, followed by a 2-stage operation. In the hands of an expert surgeon, all operations can be performed with Laparoscopic Camera Surgery (keyhole).