What is anal dysplasia?
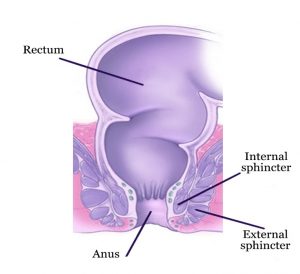
The anus is the last portion of the large bowel [Figure 1]. It is a short tube surrounded by the sphincter muscles (internal and external) which provide control of bowel motion. The lining of the anus or surrounding skin can become abnormal and give rise to anal dysplasia (a precancerous condition). When untreated anal dysplasia can lead to Anal Cancer. Anal cancer arises when the normal cells lining the anus or surrounding skin divide and grow without stopping. Anal cancer occurs in both genders but about two-thirds of patients are women. The number of anal cancer cases is on the rise in the USA and worldwide.

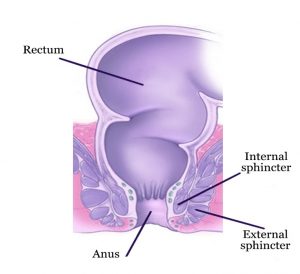
Figure 1 – The anus with surrounding internal and external sphincter muscles
What causes anal dysplasia?
The human papilloma virus (HPV) is the most common risk factor for anal dysplasia. There are many different types of HPV which are typically sexually transmitted. The majority of patients with HPV have no symptoms but some develop anal dysplasia. It is important to note that a person can become infected with HPV even without sexual activity. Coming in direct contact with an infected person and then touching the anal or genital area can transmit HPV. Risk factors for developing precancerous changes include the following: anal sex, sexually transmitted disease, numerous sexual partners, smoking, weakened immune system (such as in patients with organ transplantation, on chemotherapy, or with the diagnosis of human immunodeficiency virus). Women with prior history of HPV of the cervix are also at risk of developing anal dysplasia.
What are the symptoms of anal dysplasia?
Patients with anal dysplasia can be discovered during a routine anal examination or can present with any of the following symptoms: anal pain, itching, a non-healing rash or ulcer, a lump, drainage and discharge, and rectal bleeding. It is important to note that patients with anal dysplasia are often misdiagnosed and treated for hemorrhoids with a delay in diagnosis.
How is anal dysplasia diagnosed?
The history and physical examination are important in making the diagnosis of anal dysplasia. It is important to seek expert care. An office-based examination includes visual inspection of the skin, finger palpation of the anus, and Anoscopy or Proctoscopy to look inside the anus and rectum. In some patients, examination of the genitalia and mouth is advisable. Any suspicious lesion is biopsied. This can be done as an office-based procedure but in some patients the biopsy and examination are performed in the operating room under an anesthetic. Colonoscopy is advisable in some patients to check the rest of the large bowel.
How is anal dysplasia treated?
When the diagnosis of anal dysplasia is confirmed on biopsy, patients who are initially evaluated and biopsied in the office can require an operation under anesthetic to completely assess the anus through specialized techniques and to remove all abnormal tissue. Depending on the location and the extent of the disease, additional medical and surgical treatment may be needed in the office or the operating room especially in the immunosuppressed patients who are at risk for recurrence.
Anal dysplasia requires highly specialized care and should only be treated by physicians with expertise in the treatment of this condition. Patients with anal dysplasia should be followed closely initially, every 4 to 6 months the first couple of years, and then yearly for life. In between follow-up appointments, the patient should seek earlier evaluation if any new symptoms arise. All patients with anal dysplasia are at risk for recurrence.
What preventive measures or screening is available?
Any patient with anal symptoms should get checked by a properly trained proctologist. Screening for anal dysplasia and cancer include visual inspection, finger palpation of the anus, and Anoscopy or Proctoscopy to look inside the anus and rectum. Specialized techniques such as high resolution anoscopy and biopsy are reserved for a subgroup of at-risk patients.
Having protected sexual intercourse and limiting the number of sexual partners can decrease the risk of HPV transmission. Vaccination against HPV can be helpful but is not a guarantee against developing anal dysplasia as the currently available vaccines cover just a few of the HPV types. In order for the vaccination to have any effectiveness, it has to be administered before engaging in any sexual activity. Once infected with HPV, the vaccine may not yield any benefit. Smoking cessation is advisable in patients to decrease the risk of progression from HPV infection to anal cancer.
Why is it important to seek expert care with a board certified proctologist and colorectal surgeon?
Anal dysplasia treatment requires significant medical and surgical expertise. Only a minority of doctors have the proper training to screen and treat this condition. Often patients are incorrectly diagnosed with hemorrhoids and treated as such with significant delay in diagnosis. Early diagnosis of anal dysplasia is very important in controlling this condition.

Dr. Maher Abbas is an expert in the treatment of diseases of the colon, rectum and anus. With over a 30-year career in the USA, he has completed advanced surgical training and is American Board Certified in Colon and Rectal Surgery. Dr. Maher Abbas is a Fellow of the American Society of Colon and Rectal Surgeons.
If you would like to schedule a consultation with Dr. Maher Abbas to discuss your case, click here.